Disinfection and Sterilization in Dentistry
Maintaining cleanliness in dentistry is not just a guideline; it’s a fundamental pillar of patient safety. Dental sterilization ensures that every instrument is free from harmful microbes, protecting patients and dental professionals from potential infections. All dentists, hygienists, and assistants receive training in dental sterilization and infection prevention as part of their professional education. This article explores the key aspects of sterilization and its critical role in dental practice.
Key Takeaways
Sterilization Kills All Microbial Life: Instruments used in the mouth are sterilized to eliminate all germs, ensuring patient safety.
Different Tools, Different Protocols: Tools are categorized by their use—critical, semi-critical, and non-critical—with corresponding sterilization requirements.
Advanced Methods Ensure Safety: Heat sterilization, chemical soaking, and other methods eliminate pathogens effectively.
Team Responsibility: Dental assistants handle sterilization, while dentists oversee compliance with safety protocols.
Prevention is Paramount: Proper sterilization prevents cross-infections and ensures a safe dental experience for everyone.
Why Is Dental Sterilization Crucial?
Dental procedures inherently involve exposure to blood and saliva, creating potential pathways for infections. According to Dr. Amir Guorgui BSC, DMD, MACSD, “Sterilization is the backbone of infection control. Without it, even routine cleanings can become hazardous.”
The Centers for Disease Control and Prevention (CDC) emphasizes that maintaining proper sterilization practices significantly reduces the risk of transmitting illnesses, ensuring a safe environment for patients and staff.
By adhering to these guidelines, dental clinics can eliminate microbial contaminants on tools and surfaces, reducing the risk of cross-contamination and ensuring a safe, hygienic environment for patients and staff. This meticulous approach is not just about compliance but also about fostering trust and safety in dental care.
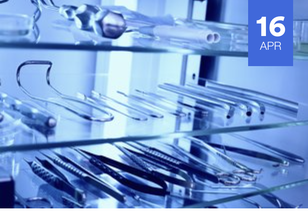
Sterilizing Dental Tools
Dental sterilization means eliminating all microbial life, including bacteria, viruses, fungi, and spores, from reusable instruments to prevent cross-contamination between patients. While some dental tools, such as disposable needles and certain plastic items, are designed for single use and discarded immediately after a procedure, many critical instruments—such as scalers, forceps, and handpieces—must be sterilized for reuse.
Dental sterilization is crucial because the human mouth harbours many microorganisms, some of which can cause severe infections if transferred from one patient to another. By ensuring that all reusable tools are sterile before each use, dental practices minimize infection risks and uphold the highest standards of patient care.
Types of Instruments
Critical Instruments: These tools, such as scalpels and scalers, penetrate soft tissue or bone and require stringent sterilization.
Semi-Critical Instruments: Items like mouth mirrors and impression trays contact oral tissues but don’t penetrate them. These also undergo full sterilization.
Non-Critical Instruments: These only touch intact skin and are disinfected rather than sterilized.
The Sterilization Process
Step 1: Cleaning
Before sterilization, all instruments undergo a thorough cleaning process to remove visible debris, blood, and saliva, which can harbor microorganisms. This step is crucial because organic matter can shield microbes from the sterilization process, rendering it ineffective. Cleaning typically involves:
Manual Scrubbing: Using brushes and detergents to physically remove debris from tools. Care is taken to avoid splashing or injury during this process.
Ultrasonic Cleaning: Instruments are placed in a specialized ultrasonic cleaner that uses sound waves to agitate a cleaning solution, effectively loosening and removing particles from hard-to-reach areas.
Rinse and Dry: After cleaning, instruments are rinsed with water to remove residues and then thoroughly dried to prevent interference during sterilization.
Step 2: Sterilization
Once cleaned, instruments are subjected to one of several sterilization methods, depending on their material and design:
Steam Sterilization (Autoclaving)
Process: Instruments are placed in an autoclave, a sealed chamber where pressurized steam reaches temperatures of 121–134°C (250–273°F).
Effectiveness: This method destroys all microorganisms, including heat-resistant spores, making it the gold standard for sterilization in dentistry.
Application: Used for metal tools like scalers, forceps, and handpieces that can withstand high temperatures and moisture.
Dry Heat Sterilization
Process: Instruments are exposed to high temperatures (160–180°C or 320–356°F) in a dry heat sterilizer for a set duration.
Effectiveness: Ideal for items that could corrode in moist environments or are steam-sensitive.
Application: Suitable for glassware, some metals, and instruments without plastic components.
Frequency of Sterilization
Instruments are sterilized immediately after each use to prevent any chance of cross-contamination. The CDC mandates that dental offices follow stringent protocols, which include:
Sterilization After Every Use: Tools are never reused without cleaning and sterilization.
Monitoring and Validation: Offices must use indicators, such as biological or chemical monitors, to confirm that sterilization cycles are effective.
Storage Protocols: Once sterilized, tools are stored in sterile packaging until needed, ensuring they remain contamination-free.
This rigorous adherence to sterilization protocols guarantees that every patient is treated with tools as safe and hygienic as brand-new instruments.
Modern Technologies in Sterilization
Advances in sterilization technology have made processes faster and more effective. Automated cleaning devices and modern autoclaves ensure precision and consistency. Incorporating these technologies further enhances safety standards.
Canadian Research on Dental Sterilization
A study published by the Canadian Dental Association (CDA) highlights the effectiveness of advanced sterilization protocols in preventing cross-contamination in dental practices. The research analyzed over 100 dental offices across Canada and found that adherence to rigorous sterilization methods significantly reduced the transmission of pathogens. The study emphasized the importance of regular staff training and the use of cutting-edge sterilization equipment to maintain patient safety.
Dr. Rob Eisen DD, notes, “Canadian research consistently shows that dental offices adhering to strict sterilization protocols provide a safer environment for patients and staff alike. This reinforces the need for ongoing education and investment in high-quality equipment.”
How Patients Can Ensure Safety
Patients can play an active role by:
Asking about sterilization protocols during visits.
Observing whether instruments are opened from sealed packaging.
Noting the overall cleanliness of the dental office.
Frequently Asked Questions
Q: How do I know if instruments are properly sterilized?
A: Sterilized tools are typically sealed in autoclave packaging that is opened before the patient. Additionally, reputable dental offices adhere to CDC guidelines.
Q: Are disposable tools safer than sterilized ones?
A: Both are equally safe when used correctly. Disposable tools eliminate the need for sterilization, while reusable tools undergo thorough cleaning and sterilization.
Q: What happens if an office doesn’t follow proper sterilization protocols?
A: Failure to sterilize tools can lead to infections and potential legal consequences for the dental practice.
Q: How do dental offices ensure that sterilization equipment is working properly?
A: Offices use sterilization monitoring techniques such as biological, chemical, and mechanical indicators to ensure sterilizers are functioning effectively.
Q: How long does the sterilization process take?
A: The time varies depending on the method. Steam sterilization typically takes 15-30 minutes, while chemical sterilization may take several hours.
Q: Do dental offices clean non-critical items like chairs and counters?
A: Yes, non-critical surfaces are disinfected between patients using EPA-approved disinfectants to ensure a clean and safe environment.