Signs Your Wisdom Teeth Are Impacted and Need Removal
Key Takeaways
- Impacted wisdom teeth can cause pain, swelling, jaw stiffness, and even bad breath.
- Wisdom tooth pain feels different than a cavity or TMJ disorder — usually involving deeper pressure and radiating discomfort.
- Removal is recommended when pain persists or leads to complications such as infection, cysts, or nerve involvement.
- Early diagnosis can help prevent serious dental and facial issues.
What are the most common signs of impacted wisdom teeth?
You're brushing, flossing, and doing everything right — but suddenly, there's an ache in the back of your mouth. Could it be an impacted wisdom tooth? The signs can be subtle at first, but they tend to escalate quickly.
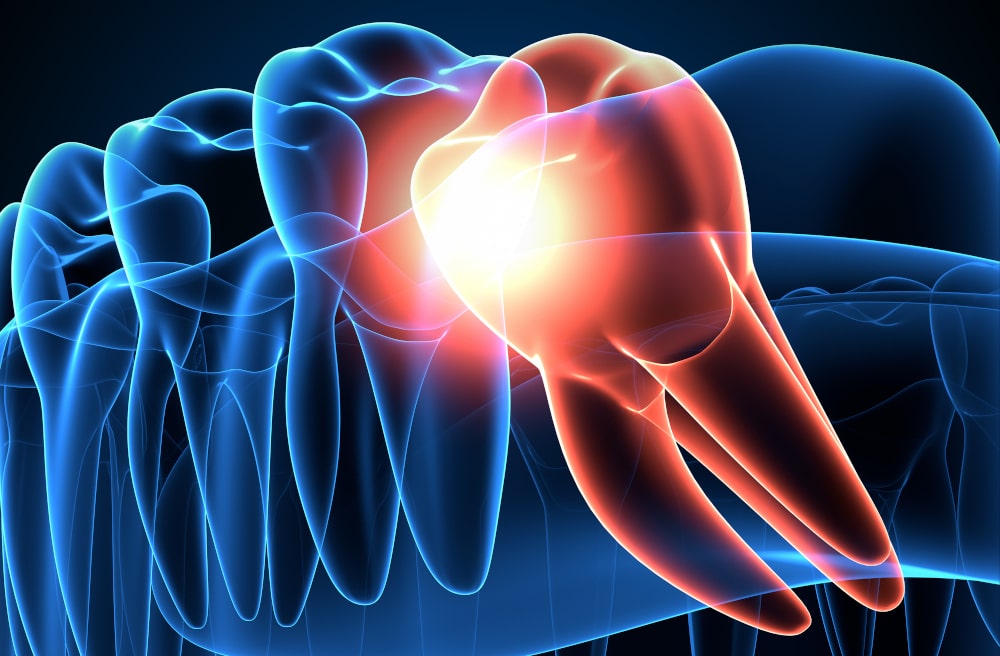
An impacted wisdom tooth occurs when there isn’t enough room for it to erupt properly, leading to partial emergence or remaining trapped beneath the gum line.
Common Symptoms to Watch For
- Pain at the back of the mouth – Often deep, throbbing, or intermittent. It may spread to nearby teeth.
- Swelling around the gums or jaw – Inflammation is your body's reaction to infection or pressure from the trapped tooth.
- Jaw stiffness or difficulty opening the mouth fully – Caused by swelling or muscle tension.
- Bad breath or unpleasant taste – Often due to trapped food and bacterial growth around partially erupted teeth.
- Red or swollen gums – Especially around the molar region.
- Headaches or earaches – Radiating pain can be mistaken for tension headaches or inner ear issues.
Additional Clinical Indicators
In some cases, the signs are more than just discomfort:
- Fever or pus may indicate an infection, such as pericoronitis.
- Swollen lymph nodes – Sign of systemic inflammation.
- Tooth crowding – Adjacent teeth may shift due to pressure from impacted wisdom teeth.
Diagnostic Tools
Dental professionals use panoramic X-rays to assess:
- The angle of tooth impaction (horizontal, mesial, vertical, distal)
- Root development
- Proximity to the mandibular nerve or sinus cavity
How does wisdom tooth pain typically feel compared to other dental issues?
Tooth pain can be confusing. It’s all in your mouth, right? But the type of pain actually tells a story — and recognizing that difference can save you from unnecessary worry or delay.
Understanding the Nature of Wisdom Tooth Pain
Wisdom tooth pain tends to be:
- Dull and deep – A throbbing pressure in the back of the mouth
- Radiating – Extending to the jaw, ear, or neck
- Intermittent or triggered – Gets worse when chewing, talking, or yawning.
Compare this to:
| Type of Pain | Wisdom Tooth Pain | Cavity Pain | TMJ Disorder |
|---|---|---|---|
| Location | Back of the mouth or jaw | Specific tooth | Jaw joint or temple |
| Pain Type | Dull, radiating, pressure-like | Sharp or shooting when eating | Aching, clicking, limited movement |
| Associated Symptoms | Swelling, difficulty opening the mouth | Sensitivity to hot/cold | Jaw locking, headaches |
| Worsens With | Chewing, pressure, yawning | Sweets, cold, pressure | Jaw movement, stress |
"Wisdom tooth pain often masquerades as something else, which is why early imaging is key. Many patients don’t realize they have an impaction until we show them the X-ray." — Dr. Rob Eisen, DDS.
In short, if the pain involves the back of your jaw, worsens over time, and includes swelling or gum tenderness, it’s wise to get checked for impaction rather than assume it’s just a cavity.
When should you consider wisdom teeth removal due to pain?
Pain alone isn’t always a reason to extract a wisdom tooth — but persistent or escalating symptoms definitely are. According to a report by the Canadian Association of Oral and Maxillofacial Surgeons, untreated impactions can lead to serious complications.
When Pain Is a Red Flag
- Chronic pain that doesn’t subside
- Recurring infections like pericoronitis (inflammation of gum tissue around the tooth)
- Cysts or tumours form near the impacted area.
- Visible damage to neighbouring teeth due to pressure
- Nerve compression or tingling sensations in the lower lip or chin
Delaying treatment increases the complexity of surgery and recovery time. For example, older adults are at higher risk for root entanglement with the mandibular nerve, which raises the chances of post-operative numbness.
What symptoms suggest your wisdom teeth might be infected?
An impacted wisdom tooth is one thing — but once it becomes infected, the stakes get higher. Infections can spread rapidly, transforming mild discomfort into a medical emergency if left untreated.
Warning Signs of Infection
- Swelling in the gums or face – A visible puffiness around the jaw or cheek area
- Red, inflamed, or bleeding gums – Especially behind the second molars
- Foul taste or bad breath – Often from pus leaking into the mouth
- Pus discharge – May appear as a yellowish fluid near the tooth.
- Fever and chills – Indicating systemic infection
- Difficulty swallowing or opening the mouth – Due to swelling of the surrounding tissue
How do dentists diagnose impacted wisdom teeth?
Unlike a regular cavity, you can’t just "look and see" if a wisdom tooth is impacted. Diagnosis involves a mix of clinical evaluation and imaging.
Key Diagnostic Tools
| Method | Description |
|---|---|
| Panoramic X-rays | Offers a full view of the upper/lower jaws and sinuses to assess impaction |
| Intraoral exam | The dentist checks for swelling, gum flaps, and signs of partial eruption |
| Cone Beam CT | Used for complex cases to evaluate proximity to nerves |
| Symptom checklist | Pain, difficulty chewing, headaches, gum infection, and jaw tightness |
Dentist's Approach
During a routine checkup, the dentist will look for:
- Alignment of third molars
- Redness or swelling near the molar area
- Presence of pericoronal flaps (gum tissue over the tooth)
They may ask questions like:
- “Do you have pain when chewing or opening wide?”
- “Has your jaw felt stiff or swollen lately?”
For patients experiencing pain, imaging typically happens immediately. This enables faster decision-making — whether to monitor or proceed with surgical removal.
How long does it take to recover after wisdom tooth removal?
Post-surgery recovery from wisdom tooth extraction isn’t as daunting as many think — provided you follow the instructions carefully.
General Healing Timeline
- First 24 hours: Blood clot forms; swelling begins
- Days 2–3: Swelling peaks; mild bruising may occur
- Days 4–7: Swelling reduces, pain subsides
- Week 2: Stitches (if present) removed; most discomfort resolved
- Weeks 3–4: Full tissue healing
Day-by-Day Recovery Plan
| Day | What to Expect | Tips for Comfort |
|---|---|---|
| Day 1 | Bleeding and swelling start | Apply ice packs, bite on gauze |
| Day 2-3 | Peak swelling, mild pain | Take prescribed pain meds, soft diet |
| Day 4-5 | Swelling goes down | Rinse gently with salt water |
| Day 6-7 | Bruising may fade | Resume light activity |
| Week 2 | Almost normal, minor tenderness | Avoid hard foods, continue oral hygiene |
Tips to Accelerate Healing
- Avoid smoking and alcohol – They disrupt clot formation
- Stay hydrated – But skip the straws (suction can dislodge a clot)
- Stick to cold and soft foods, such as yogurt, smoothies, and applesauce.
- Elevate your head – Reduces swelling.
- Apply ice for the first 48 hours, then switch to warm compresses.

Is wisdom tooth extraction painful during and after the procedure?
Many patients fear the pain of wisdom tooth removal, but the reality is far more manageable than anticipated. Thanks to modern anesthesia and pain management techniques, most people experience minimal discomfort during the procedure and only moderate pain during recovery.
During the Procedure
You’re not expected to feel pain — just pressure. That’s because dentists and oral surgeons typically use one of the following anesthesia options:
- Local anesthesia (e.g., lidocaine) to numb the area
- Conscious sedation (oral or IV sedation) to reduce anxiety and memory of the procedure
- General anesthesia for complex or multiple extractions
After the Procedure
Some discomfort is expected, especially as the anesthesia wears off. Most patients describe:
- Mild to moderate pain in the first 24–48 hours
- Swelling and jaw stiffness for up to a week
- Throbbing pain if dry socket occurs (a dislodged blood clot)
Pain Management Methods
Dentists typically recommend a combination of:
- Over-the-counter medications like ibuprofen or acetaminophen
- Prescription painkillers for severe cases
- Cold compresses to reduce inflammation
- Saltwater rinses to promote healing
In short, the procedure is far less painful than the anxiety surrounding it. With proper care, most patients are back to normal within a few days.

What happens if you don’t remove an impacted wisdom tooth?
Let’s not sugarcoat this: leaving an impacted wisdom tooth untreated can create long-term dental and medical problems. Many people put off removal because the pain subsides temporarily — but the complications often grow silently.
Long-Term Risks
- Tooth crowding and shifting – Pressure from the impaction may cause other teeth to shift out of alignment.
- Cyst formation – Fluid-filled sacs can develop around the impacted tooth, causing bone loss.
- Recurring infections – Especially pericoronitis, due to partial eruption and trapped bacteria.
- Damage to adjacent teeth – Impacted teeth can erode the roots of neighbouring molars.
- Jaw stiffness or chronic pain – Especially when inflammation spreads to joints and muscles.
Expert Insight
"Impacted third molars are like ticking time bombs. They may not hurt today, but if left untreated, they often cause complications requiring more invasive treatment later." — Dr. Amir Guorgui, BSc, DMD, MACSD.
How can you manage wisdom teeth pain at home before removal?
Waiting for your dental appointment doesn’t mean you have to suffer in silence. Several home care strategies can ease pain and inflammation until your wisdom tooth can be treated.
Step-by-Step Home Relief Plan
- Rinse with warm salt water (1 tsp salt in 250 mL of warm water)
- Reduces bacteria and soothes gum inflammation
- Apply an ice pack on the affected side (15 minutes on, 15 off)
- Helps minimize swelling and numbs the area
- Take OTC pain medication like ibuprofen
- The anti-inflammatory effect reduces pressure pain
- Eat soft, cool foods (yogurt, applesauce, smoothies)
- Avoid anything sticky, crunchy, or spicy
- Keep the area clean
- Gently brush and avoid disturbing partially erupted teeth
What to Avoid
- Straws – Can dislodge clots or worsen inflammation
- Smoking – Impairs healing and promotes infection
- Touching the area – Increases irritation and bacterial exposure
With consistent care, pain can be kept under control — even if removal is a few days away. Just don’t delay seeking professional help if symptoms worsen or new ones appear.

Do all wisdom teeth need to be removed?
The short answer? Not always. Not all wisdom teeth require extraction, and the decision depends on several clinical and patient-specific factors. In fact, the routine removal of symptom-free wisdom teeth has become a topic of debate in recent years.
Monitoring vs. Extraction
Dentists consider removal based on the following factors:
- Symptoms – Persistent pain, swelling, or infection
- Tooth positioning – Impacted, misaligned, or crowded neighbouring teeth
- Oral hygiene access – Difficulty cleaning the area properly
- Age and root development – Younger patients heal faster and have fewer complications
When no symptoms are present and X-rays show no impaction or pathology, monitoring may be the better choice. Regular check-ups and updated imaging are essential.
Dentist Recommendation Table
| Wisdom Tooth Status | Dentist Likely Recommends | Why? |
|---|---|---|
| Fully erupted & straight | Monitor | Easy to clean, low risk of impaction |
| Partially erupted | Remove | Prone to infection and pericoronitis |
| Horizontally impacted | Remove | High risk to adjacent teeth and nerves |
| Deeply embedded with no symptoms | Monitor (case-dependent) | Surgery risk may outweigh the benefits |
| Causing cysts or decay in nearby tooth | Remove | Urgent intervention required |
Are there any warning signs of complications after removal?
Yes — and ignoring them can delay healing or result in severe post-operative problems. Although most recoveries go smoothly, certain red flags require immediate dental attention.
Most Common Post-Op Complications
- Dry socket – Occurs when the blood clot is lost prematurely; causes intense, radiating pain
- Infection – Swelling, pus, or fever that persists beyond the third day
- Prolonged bleeding – Oozing that continues for more than 24 hours
- Swelling that worsens after 3–4 days rather than improves
- Difficulty breathing or swallowing – Could indicate spreading infection
Specification Table
| Complication | Warning Signs | What to Do |
|---|---|---|
| Dry socket | Severe throbbing pain, bad smell, exposed socket | Return to the dentist for dressing |
| Infection | Fever, pus, red gums, painful swelling | Antibiotics and follow-up exam required |
| Bleeding | Bright red blood >24 hours after surgery | Bite gauze, apply pressure, call the dentist |
| Swelling | Expanding or shifting swelling | Ice, anti-inflammatories, call the dentist |
When to Call Your Dentist
Call your oral surgeon or dentist if you notice:
- A foul taste that doesn’t go away
- Numbness beyond 24 hours
- Headache, fever, or dizziness
- Jaw locking or clicking that worsens post-surgery
What’s the final takeaway on wisdom tooth symptoms and removal?
Navigating wisdom teeth can be tricky — but knowing what to look for and when to act makes all the difference. From mild pain to serious complications, every symptom is a signal your body is giving you.
Summary Table
| Symptom/Condition | Action to Take |
|---|---|
| Dull ache in the back of the jaw | Monitor, consult a dentist |
| Swelling and redness | Schedule exam, consider imaging |
| Persistent pain/infection | Extraction often recommended |
| Fever, pus, or cysts | Urgent removal needed |
| No symptoms, fully erupted | Periodic monitoring only |
Final Recommendations
- Don’t ignore recurring jaw or gum discomfort
- Wisdom tooth pain is distinct from cavities or TMJ — pay attention to where and how it hurts.
- Get panoramic imaging before making removal decisions
- Follow post-op care precisely to avoid complications
- Always ask for a second opinion if uncertain